1-256-329-8401
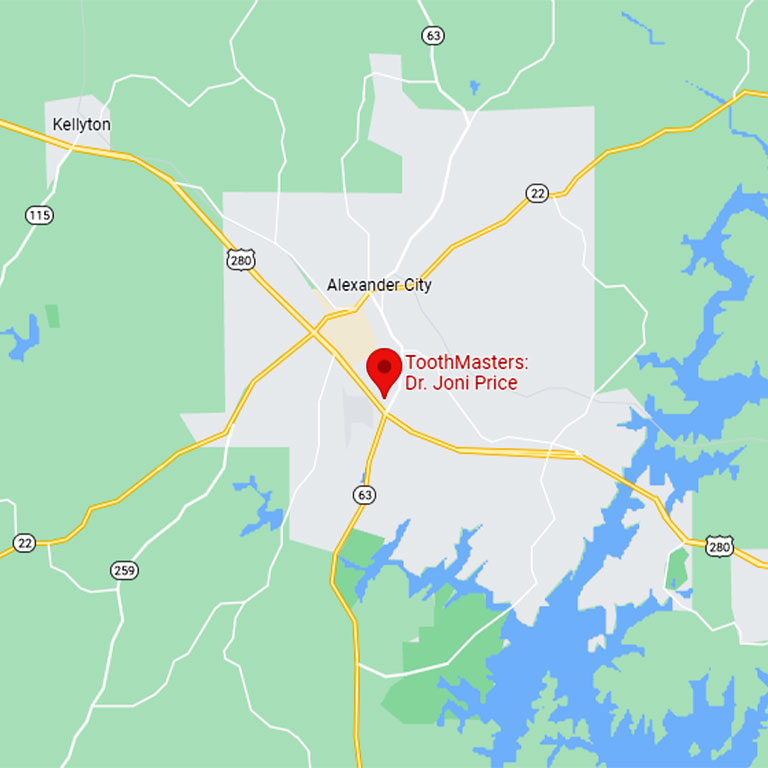
139 Aliant Parkway, Alexander City, AL 35010
info@toothmasters.com
Notice of Privacy Practices
Disclaimer
Business Hours
Monday: 8:30AM - 4:30PM
Lunch: 12:00PM - 1:00PM
Tuesday: 8:30AM - 4:30PM
Lunch: 12:00PM - 1:00PM
Wednesday: 8:30AM - 4:30PM
Lunch: 12:00PM - 1:30PM
Thursday: 8:30AM - 3:00PM
Friday: CLOSED
Saturday: CLOSED
Sunday: CLOSED